StaphBone
Staphylococcus aureus pathogenesis: from sepsis to hematogenous chronic bone infections
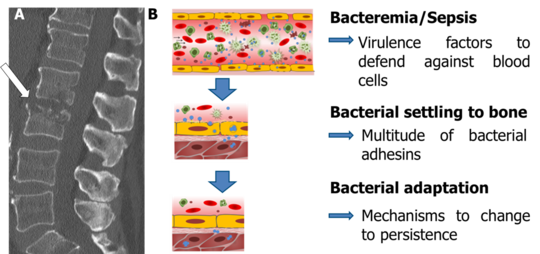
Staphylococcus aureus can colonize the epithelial surface of many healthy individuals, but is also one of the most frequent causes of sepsis. S. aureus can escape from the bloodstream and cause invasive tissue infections, such as osteomyelitis that is extremely difficult to treat. S. aureus has a multitude of virulence factors, including adhesive surface proteins (adhesins), toxins, and cytotoxic peptides. The endowment with virulence factors is strongly strain-dependent and their expression is under the tight control of complex and highly dynamic regulatory systems. Yet, defined factors responsible for hematogenous spread to bones and adaptation within host tissue have not been identified. In our study we aim to characterize clinical isolates from spondylodiscitis/osteomyelitis of hematogenous origin and compare them to isolates from sepsis without metastatic complications or from nasal colonization. All isolates will be analyzed for their virulence factor expression by molecular methods and for their infection strategies by functional assays. Raman spectroscopic typing will be carried out to identify characteristic features of different S. aureus sub-groups. The process of osteomyelitis development and the impact of bacterial regulatory and virulence factors will be further studied by testing and analyzing strains in our hematogenous murine sepsis model that develops to chronic osteomyelitis and closely mimics the human infection. Using this model, we further aim to develop novel imaging strategies (e.g., two-photon microscopy and MRI) to assess pathogenesis from sepsis to chronic osteomyelitis. The identification of virulence patterns that are required for S. aureus to develop hematogenous metastatic bone infections opens new options for preventive and therapeutic measures.